Welcome back to our continuing discussion of endometriosis. If you haven’t already, I encourage you to check out my earlier blog post for a comprehensive overview of endometriosis. Building on the principles we covered before, we’ll explore management techniques in more detail in this continuation.
Pain Management:
One of the main characteristics of endometriosis is chronic pelvic pain, and managing pain well is essential to improving quality of life. Over-the-counter pain relievers, such as paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs), can provide relief. Additionally, hormonal treatments, like birth control pills, progestogens, and GnRH analogs, play a pivotal role in managing pain by suppressing the disease activity and thus the pain symptoms.
However, understanding the potential side effects of medications is essential. Long-term use of NSAIDs could lead to stomach discomfort, while hormonal treatments might bring about side effects including acne, weight gain, headaches, and vaginal spotting. Please consult your doctor before taking any medications for a thorough evaluation.

Surgical Intervention:
For some individuals, surgical intervention becomes a viable option, particularly when symptoms are severe or fertility concerns are at the forefront. Nowadays, keyhole surgery (laparoscopy) is often used and preferred because it typically leads to a shorter hospital stay, a smaller scar, less pain, and faster recovery. Engage in open discussions with your healthcare provider to explore the surgical path and determine the most suitable approach tailored to your unique needs.

Fertility Considerations:
Having endometriosis doesn’t necessarily mean you’re infertile. Approximately 60-70% of women with endometriosis can conceive naturally. However, endometriosis can still pose challenges to fertility. If fertility is a priority, early discussions with your healthcare team are essential for determining an effective management plan.
While complications during pregnancy are rare, women with endometriosis may face a slightly elevated risk of miscarriage or ectopic pregnancy. It’s important to inform your doctor if you’re pregnant and have endometriosis, although additional monitoring is usually not necessary. Assisted reproductive technologies like in vitro fertilisation (IVF) may be recommended to increase the chance of conception. Understanding your fertility options empowers you to make informed decisions aligned with your family planning goals.
Holistic Wellness:
Endometriosis management extends beyond medical and surgical interventions, encompassing holistic well-being. Emotional support is crucial, and participating in support groups or seeking counselling can provide valuable perspectives and coping mechanisms. Embracing a healthy lifestyle with regular exercise and a balanced diet contributes not only to physical health but also to overall well-being.
The effectiveness and risks of various non-medical interventions for managing endometriosis symptoms, such as Traditional Chinese Medicine, nutrition, acupuncture, and physiotherapy, remain uncertain. Hence, no specific recommendations can be made regarding their use to alleviate pain, enhance overall well-being, or increase chances of conception. It’s advisable to consult your doctor for more information and guidance.
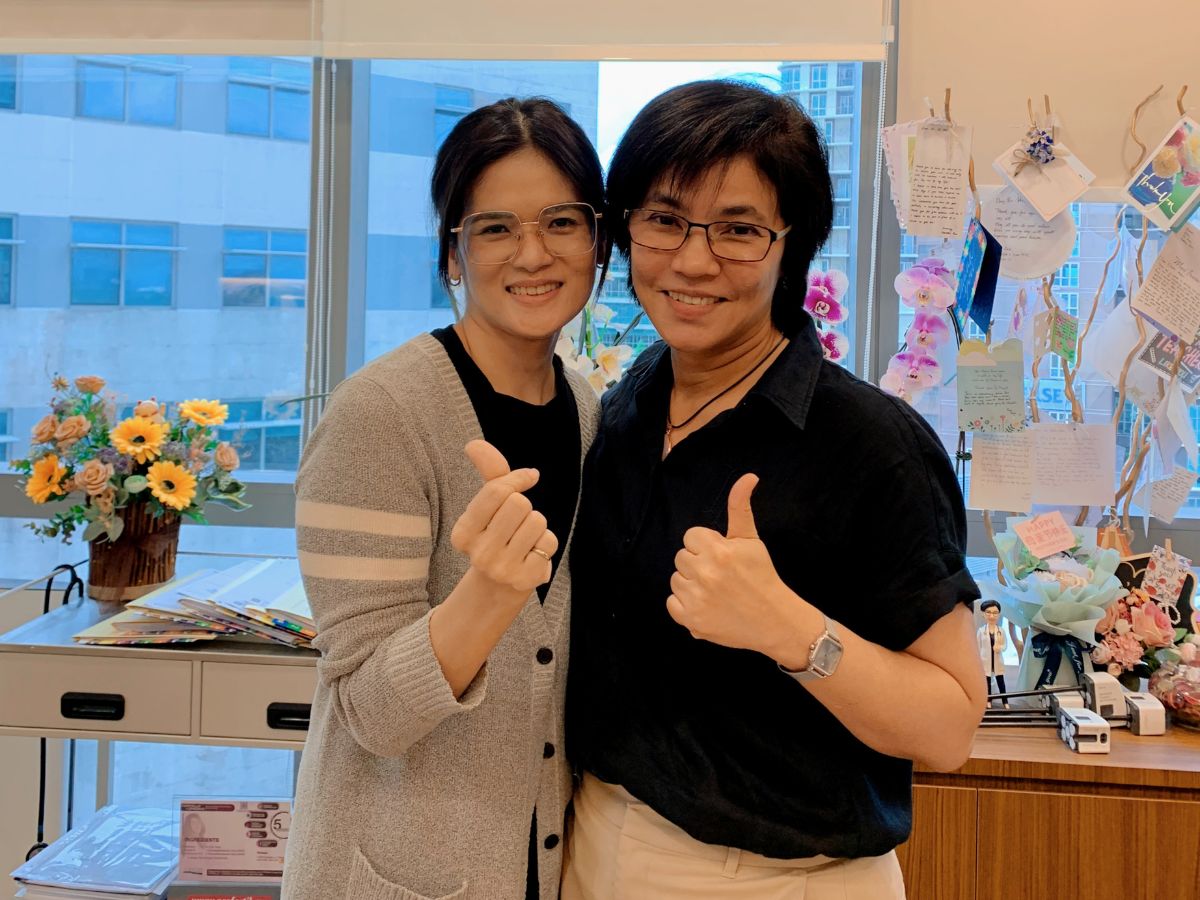
In managing endometriosis, remember your journey is unique. Communicate openly with your healthcare team, ask questions, and actively engage in decisions for better well-being. Stay informed, stay engaged, and know that you are not alone in this journey.